PEMFs and Parkinson’s (PD) Table of Contents PEMF treatment of Parkinson patient – Case Report A 74-year-old retired building inspector with a 15-year history of Parkinson’s disease (PD) presented with a severe resting tremor in the right hand, generalized bradykinesia, difficulties with the initiation of gait with freezing, mental depression, and generalized cognitive impairment despite […]
PEMFS AND BRAIN RECOVERY AFTER STROKE Table of Contents The ability to recover after stroke depends on many factors, including the regenerative capabilities of the brain. Recovery depends on the plasticity of the brain. The plasticity, or neuroplasticity, required in a damaged brain is very different from the plasticity of a normal functioning brain. The demand for adaptive […]

Urinary Stress Incontinence Improved By High Intensity PEMF Therapy Table of Contents WHAT IS STRESS INCONTINENCE? Stress incontinence, primarily urinary, is a very common problem in women of childbearing age and older. Treatment is either nonsurgical or surgical. Nonsurgical treatment includes biofeedback, vaginal cones, and electrostimulation, with success rates ranging from 9-63%, side effects and […]

Pulsed ElectroMagnetic Fields Help with Muscle Soreness After Exercise Table of Contents MUSCLE SORENESS FROM EXERCISE Delayed onset muscle soreness [DOMS] is a common painful condition that arises chiefly from exercise-induced muscle damage after unaccustomed physical activities, including intentional exercise. DOMS can happen after yardwork, snow shoveling, strenuous physical work, muscle strengthening and gym workouts. […]
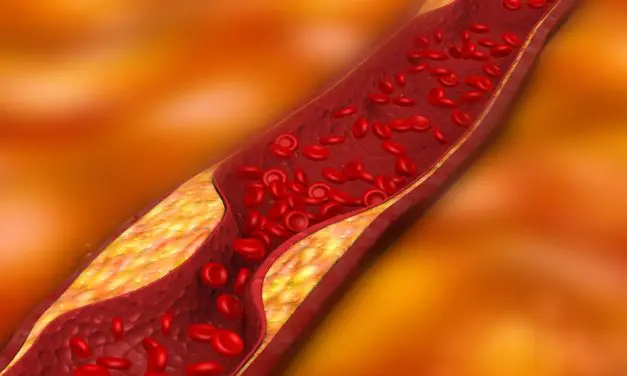
PEMFs Reduce Progression of Arteriosclerosis Table of Contents Vascular disease within the heart and throughout the body is one of the top causes of death and disability. Additionally, most vascular disease is associated with blockages of blood vessels, called arteriosclerosis or atherosclerosis. Atherosclerosis is a leading cause of vascular disease worldwide. Its major clinical manifestations […]

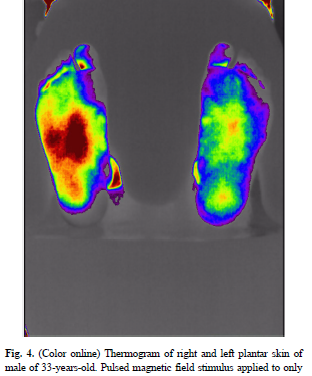
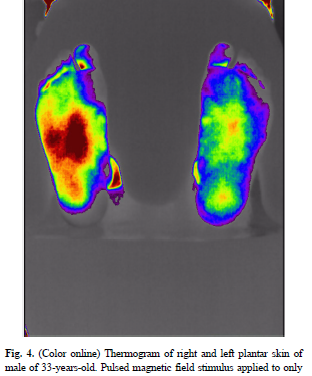
PEMFs for Healing Diabetic Foot Ulcers Table of Contents Diabetes is an increasing problem around the world. Vascular disease is one of the most common complications of diabetes. Because of this, wound healing in diabetics is a major health challenge. Short of curing and reversing diabetes, managing the complications such as foot ulcers is difficult. […]
PEMF for Microcirculation and Increasing Blood Flow Table of Contents CAN PEMFS HELP IMPROVE BLOOD FLOW AND CIRCULATION? I have previously stated that almost all magnetic fields, static and PEMF, stimulate circulation and microcirculation. Within certain limits, almost any magnetic field intensity will increase circulation. Improvements in circulation are not the limited domain of any […]

PEMFs Reverse the Muscle Damage Caused By Cholesterol Lowering Drugs (Statins) Table of Contents STATIN DRUG USE One in four Americans, ages 45 and older or almost 32 million take a statin. Statins are used to lower cholesterol into what are considered to be optimal ranges. Cholesterol is a fundamental molecule made by the body […]

Essential Tremor and Treatment with PEMF Devices Table of Contents ESSENTIAL TREMOR AND TREATMENT WITH PEMF DEVICES Essential tremor (ET) is a neurological condition that most commonly causes a rhythmic trembling of the hands while performing a task like eating, writing, dressing, drinking, or holding a posture such as holding the arms stretched out in […]

Diabetic Foot Ulcer Infections – Combining Therapy with PEMF and Lasers Table of Contents I have often said that combining PEMF therapies with other modalities produces better results than either modality alone. Likewise, I have found that if one could only afford to have one system, PEMFs would likely give the most value because of […]