PEMF'S AND BREAST IMPLANTS
Table of Contents

I am writing this blog to correct a misunderstanding about the risk of using PEMFs with breast implants, also called breast augmentation. It has been stated that PEMFs can affect the covering of the implant, possibly creating weakening. After further research, it is evident that most PEMFs create minimal risk and may in fact be helpful to reduce complications and assist with postoperative recovery.
BREAST IMPLANTS ARE COMMON IN THE UNITED STATES
According to the American Society of Plastic Surgeons (ASPS) statistics for 2017, breast augmentation was performed on 300,000 women. Breast augmentation continues to be the top cosmetic surgical procedure and has been since 2006. Silicone implants were used in 87% and saline implants in 13% of all breast augmentations in 2017. Breast augmentations increased and implant removals decreased between the years 2000 and 2017, indicating increased popularity of these procedures. Breast augmentation numbers were 212,500 in 2000 and 300,378 in 2017 – a 41% increase in procedures. Breast implant removals were 40,787 in 2000 and 27,507 in 2017 – a 33% reduction in removals.
ASPS doctors are not the only ones who do breast implants, which means even more procedures are performed than stated above. There is a recent estimate of over 550,000 breast implants placed per year. (Doren) This may amount to almost 4 percent of women in America, or one in every 26 women, has breast implants. The world’s first breast implant surgery was performed in Houston, Texas, in 1962. (Mona) 894,206 U.S. women had cosmetic breast implants between 1963 and 1988. It is currently estimated that about 10 million women have had breast implant surgery. Of these, about 75% involved cosmetic enhancements, and 25% involved reconstruction after mastectomy.
Silicone breast implants have been available in the U.S. since 1963 and saline implants became available in the 1970s. (Brown) 20% of implants have been used for reconstruction or other medical purposes and 80% were for cosmetic augmentation.
ADVERSE EVENTS WITH BREAST IMPLANTS
In 1992–1993, the FDA received a flood of 50,185 adverse event reports on silicone-gel breast implants
from implant manufacturers and others. Of the 94,120 adverse event reports on silicone-gel breast implants sent to the FDA between 1984 and 1995, 27% reported implant rupture and an additional 10% reported implant (capsular) contracture, the stiffening of scar tissue that can lead to pain and rock-hard, misshapen breasts.
One population-based study (Doren) described local complications that resulted in additional surgeries. In this study, during a short follow-up period with a mean of 7.8 years, 28% of women underwent at least one additional surgery. The most frequent reason for the added surgery was capsular contracture (18%), and women with mastectomies were more likely to have complications leading to re-surgeries than women having implants for cosmetic augmentation.
Another study reported on 15 years of experience with 482 patients with saline and 330 patients with silicone implants. (Codner) The most common complications included capsular contracture, rippling, rupture, infection, and hematoma. A total of 8% of patients developed grade III/IV capsular contracture by 6 years. The raw incidence of rippling was 7%. The rate of total reoperation at 1 year was 14%.
Rupture or deflation occurs in roughly 10-25% of silicone gel and saline implants over 10 years. Capsular contracture happens in 18-19% of both types of implants over 10 years. Contracture and rupture risk appears to vary with the manufacturer.
Silicone breast implants have been available in the United States for more than 30 years, but there are still questions about their safety and effectiveness. Their safety has been debated extensively, even resulting in a temporary ban (1992-2006) by the FDA on silicone-gel implants for cosmetic indications. The FDA has fewer concerns today about an association between breast implants and connective tissue disease or breast cancer than in 1992 because of epidemiologic studies that have addressed these questions.
Because of persistent concerns, per the FDA, even if there are no symptoms, women with breast implants should have a first ultrasound or MRI at 5-6 years after the initial implant surgery and then every 2-3 years thereafter. If there are symptoms at any time or uncertain ultrasound results for breast implant rupture, an MRI is recommended. If the implants are placed for cosmetic reasons, it is possible that health insurance will not cover these tests. (FDA)
COMPLICATIONS FROM BREAST IMPLANTS
Because of problems with breast implants patients may not only need to have additional surgeries, but the implants may also need to be removed. In 2013 alone, there were 23,770 breast implant removals.
Per an FDA database, risks of breast implant surgery may include:
- breast pain (36.5% of procedures),
- skin or nipple-areola sensitivity changes or loss (35% of procedures),
- asymmetry (28% of procedures),
- impact of aging or weight change on size and shape of the breast (10% of procedures),
- infection requiring possible removal of implant (9% of procedures),
- swelling (9% of procedures),
- scarring (7% of procedures),
- fluid collections (seroma) (6.5% of procedures),
- hematoma (2.8% of procedures),
- tissue death of breast skin or nipple (2% of procedures),
- inability to breastfeed (1.6% of procedures),
- complications of anesthesia (1% of procedures),
- bleeding,
- chronic pain,
- damage to surrounding tissue, such as muscle, nerves, and blood vessels
What IS CAPSULAR CONTRACTURE AND WHAT CAN BE DONE ABOUT IT?
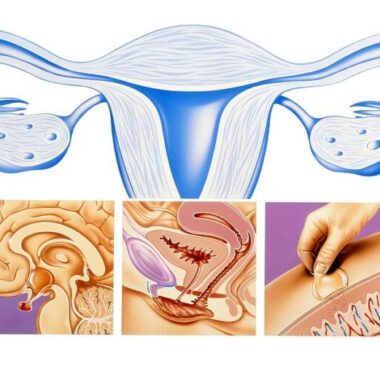
The body normally reacts to any foreign object inside it by trying to isolate the object by creating a barrier or “capsule” of scar tissue around it. This reaction is natural and depends on the individual body’s degree of reaction. The scarring is made up of connective tissue. Connective tissue varies greatly from one person to another, as does the healing process. Some people develop thick or inflamed scar tissue after any kind of skin injury while others have barely visible scars.
Foreign bodies generate immune reactions, and these can be local or systemic. As with scar healing, immune reactions vary tremendously from mild to severe. Inflammation is a common denominator to all healing. Acute inflammation is necessary for healing, but it may be exaggerated. Chronic inflammation is undesirable and damaging to the body. The goal is to prevent exaggerated acute healing and reduce chronic inflammation.
Women who are prone to developing aggressive scar tissue should consider avoiding elective, cosmetic plastic surgery. Those who have compromised immune systems or autoimmune diseases should strongly consider avoiding having elective breast augmentation.
The scar tissue “capsule” around any kind of implant (medical or cosmetic) is normal. The capsule helps to keep the breast implants in place, preventing slippage. In some women, this capsule becomes hard and starts to contract around the implant. This can cause changes to the shape of the breast and, less commonly, pain in the breast. Research shows that about one in six breast augmentation patients experience some degree of capsular contracture, though not all produce obvious symptoms.
The severity of capsular contracture is rated using a grading system:
- Grade 1: Firstly, grade one capsular contracture is asymptomatic (producing or showing no symptoms). The formation of scar tissue around the implant does not interfere with the size, shape, or texture of the breasts. The breasts look natural and remain soft to the touch.
- Grade 2: Secondly, grade two capsular contracture usually presents itself with only minor cosmetic symptoms. The breasts will usually appear normal in shape but feel somewhat firm to the touch.
- Grade 3: Thirdly, grade three capsular contracture presents itself with obvious cosmetic symptoms. The breasts will be firm to the touch and appear abnormal, e.g., they will be overly round, hard-looking and the nipples may be misshapen. However, this grade of capsular contraction often doesn’t cause much (if any) pain.
- Grade 4: Fourthly, like grade three capsular contracture, grade four capsular contracture causes the breasts to become hard and misshapen. Patients with grade four capsular contracture also experience breast soreness; their breasts will often be tender and painful to the touch.
Generally, capsular contracture occurs during the healing process. About 75% of all contractures occur within two years of the implants being placed, but it can also occur many years after. If there is a contracture, the implants should be checked for ruptures. Ruptured implants are the most common cause of late-onset capsular contraction. Ruptures are best detected by MRI or ultrasound.
Contracture is not caused by breast implants being in any way toxic or dangerous. Saline implants contain only saline solution, which can be safely reabsorbed by the body with no ill effects. Silicone gel implants are made of medically inert silicone. Capsular contracture is not usually dangerous to health unless the implants have ruptured. Rupture of gel implants can sometimes lead to infection.
Researchers believe genetics play a role in who develops capsular contraction and who does not. If you have a family history of autoimmune disease or have relatives who frequently develop thick scar tissue after injury (or who have had difficulties with medical implants), then you may have a slightly heightened risk of developing this condition. However, it’s impossible to accurately predict who will develop a “random” case of capsular contracture (i.e., one that is not caused by any identifiable external factors) and who will not.
Medical conditions that affect the body’s ability to heal can increase the risk of post-op problems, including:
- diabetes;
- connective tissue disorder;
- active smoker or a former smoker;
- currently taking drugs that weaken the body’s natural resistance to diseases, such as steroids and chemotherapy drugs (e.g., prednisone, tacrolimus, sirolimus, mycophenolate, azathioprine, cyclosporine, methotrexate, chlorambucil, leflunomide, or cyclophosphamide); or
- history of chemotherapy, planned chemotherapy, history of radiation therapy, or planned radiation following breast implant placement.
Hematomas and seromas (blood clots that sometimes form after surgery) may also increase the risk of capsular contracture. These blood clots provide a rich supply of blood nutrients for bacteria, thereby encouraging the growth of biofilm.
Besides implant ruptures, research is showing that “biofilm” often leads to the development of contracture. Biofilm is a thin layer of bacteria that develops around implants after bacteria (often staph) is introduced to the breast cavity during surgery. These bacteria cause a chronic, low-grade infection that may not produce noticeable symptoms (such as fever or severe fatigue). The body’s response to this chronic low-grade infection is to produce more and more fibrous scar tissue, eventually leading to capsular contracture.
BIOFILM AS A CAUSE OF CONTRACTURE
Bacteria that cause implant-related infections, whether with implanted medical devices or breast implants, live in well-developed biofilms. Biofilm is a non-moving microbial community characterized by microbial cells that are irreversibly attached to a surface or to each other, embedded in a matrix of various very large molecules(macromolecules) composed of many repeating subunits (polymers) they have produced. Slime on a pond surface is a good visible example.
Biofilm production was shown by a recent study conducted on pigs implanted with medical-grade silicone implants. (Tehrani) Pigskin is frequently used for research because it is so similar to human skin. Pigs who had staph bacteria on their skin at the time of implantation had a significant increase in getting capsular contracture. The surgical environment is aseptic, so that is unlikely to be the cause. Some people are natural carriers of staph bacteria, always having it on their skin and having no symptoms. Only when their skin is cut do these bacteria have a chance to cause problems. It’s not always possible to eliminate 100% of the bacteria that are present even with adequate prepping for surgery.
Important risk factors for biofilm development include immunomodulation/steroid therapy, diabetes, smoking, and renal disease/hemodialysis-findings that point to a critical role of a compromised innate immune response in determining vulnerable subpopulations. (Stewart)
IMPLANTS AS PART OF RECONSTRUCTIVE SURGERY
Women undergoing reconstructive breast surgery following a mastectomy, usually for cancer, undergo a multiphase process. The 1st stage is to create a pocket for an eventual implant. In this stage an expander is placed into the breast with a port, which is often metal, allowing expansion of this chamber gradually over time to stretch the overlying skin of the breast area to accommodate an implant. In a subsequent stage, an expander is replaced with a permanent implant.
MRIs of the breast done during the 1st stage may create heating issues with metallic ports. Cautionary measures are used to reduce the risk of health problems when MRIs are necessary. (Marano; Thimmappa) Capsular contractions can occur in these post-reconstructive as well. High-frequency PEMF therapy has been used successfully in helping to control the problem, to retain the implant, along with other surgical approaches. (Silver)
How CAN CAPSULAR CONTRACTURE BE PREVENTED?
Surgeons use various approaches to reduce the potential for developing contractures. However, they cannot be avoided completely. (Tehrani) This is where PEMFs come in. Medium to higher intensity PEMFs applied locally can reach deep enough into the breast to prevent the tissues around the implant from aggressively forming scarring as well as reducing biofilm.
USING PEMF’S WITH BREAST IMPLANTS
Ideally, a woman intending to have breast implants should do pretreatment with PEMFs to reduce the burden of staph or other bacteria on top of or buried in the skin. In addition, PEMFs have been found to increase stress proteins and stem cells in the tissues that would be traumatized by the surgery. This would protect those tissues and reduce the degree of stress response from the surgery as well as stimulating growth factors and stem cells to initiate appropriate healing. PEMFs have been found to reduce aggressive scar formation as well.
PEMF therapy would be safe and effective even in women having reconstructive breast implants following mastectomies or other breast surgeries. In fact, it may be even more helpful in this setting because of the extent of surgical trauma in these women.
Once the surgery is completed, PEMF therapy can be used daily during the post-surgery healing process and for the next 2 years to reduce the risk of developing capsular contracture as well as helping with breast or chest pain, loss of breast or nipple sensation, wound healing, resolution of any hematomas or seromas, and postoperative infections.
If PEMF therapy is not initiated before or soon after surgery, it could be useful for helping with the early grades of capsular contracture. Grade four cases may require more aggressive surgical intervention in addition to PEMFs. Again, medium to higher intensity PEMF therapy systems would provide the best results. See the blog about PEMFs for reducing inflammation.
Since a large proportion of breast implants done now are placed under the chest muscles the distance from the skin on the surface of the breasts to the back of the implant is farther than implants placed within the breast. All of this will vary with the cup size. The possible distance could be 2-8 inches or more, measured through the center of the implant. It may be best to do this measurement when laying on the back.
To deliver the optimal intensity to reduce inflammation for 2 inches depth would require a PEMF intensity of almost 500 Gauss; for 4 inches depth would require a PEMF intensity of almost 2000 Gauss. For 8 inches depth, the intensity would need to be about 6000 Gauss. It is not recommended to use a magnetic field of sufficient intensity to cause muscle contractions of the chest wall or pectoral muscles. To view device options, go here.
SAFETY OF PEMF’S WITH BREAST IMPLANTS
MRI is routinely used to diagnose breast issues. It is used for screening for cancer and with breast implants for contracture and rupture. MRI uses high intensity and high-frequency magnetic fields with no reported issues of heating or damage to the breast implants. Problems with the use of MRI are typically only found in the setting of inflatable breast expanders with metal ports. If the MRI magnetic field intensity is kept under 1.5 Tesla, problems with heating of the metal ports are eliminated. None of the PEMF systems recommended for treating breast issues, including those surrounding breast implants, are of equivalent intensity or frequency. Most high-intensity PEMF systems used in this capacity are under 1 Tesla peak intensity. Additionally, the frequencies are rarely over 100 Hz (or <100 pulses per second).
PEMFs AND BIOFILM CONTROL
Specific ultrasound waves therapy has been shown to increase the effectiveness of antibiotics in combating biofilm. (Tehrani) Similarly, PEMFs have been shown to be effective in dealing with infections that are part of biofilms and enhance the value of antibiotics if needed. (Pawluk).
LONG TERM RISKS OF IMPLANTS, INCLUDING BREAST CANCER
Furthermore, PEMFs have the advantage of being able to be used at home daily both for treatment and prevention. As mentioned earlier, the best scenario would be to own a PEMF system and begin treatment before an implant, continue use after the surgery, and then ongoing for at least 2 years to reduce the risk of contracture. Because of the risk of long-term rupture after contractures have happened, PEMF therapy may be valuable longer-term. PEMF therapy may even prevent the development of non-implant-related breast cancer. Inflammation in the breast increases the risk, even without implants.
A major review of studies looking at whether implants may cause breast cancer concluded that women who have undergone cosmetic breast implantation do not have an increased risk of breast cancer. (Noels) This appears to be true for silicone implants (Frame) However, there are increasing reports of anaplastic large-cell lymphoma (ALCL), extremely rarely, associated with any silicone implant, especially textured silicone implants, particularly those textured using salt extraction technology. (Frame) the number of women with implants needed to cause 1 breast-ALCL diagnosis before the age of 75 years, was 6920. ALCL risk increased because of a local inflammatory response, elicited by silicone-derived products or specific bacterial species adherent to the prosthesis surface (biofilm), possibly creating an auto-immune response. (de Boer) So, inflammation around the implant is possibly implicated.
Summary
Breast augmentations or implants are the number one cosmetic procedure performed since 2006, with about 300,000 being performed annually as of 2017. Complications and adverse events are relatively common. As a result, as many as 28% of women need at least one additional surgery. Infection requiring possible removal of the implant happens in 9%. Contractures of the breast implant capsule occur at the rate of about 18%.
Infections, biofilm development, and contractures are usually related to inflammation due to the implant being a foreign body. Bodies react to implants in different ways, some more aggressively than others.
Lastly, PEMF therapy used before, at the time of surgery, and for several years following augmentation can be used to reduce the likelihood of breast implant complications by decreasing inflammation and helping the body fight any incidental infections. If PEMF therapy is started after problems have begun, the potential benefit of the PEMFs may be reduced, and take longer to see results. So, the sooner PEMF therapy is started when problems begin, the better the results should be. The intensity of the magnetic field should be a minimum of 100 Gauss to be able to at least minimally affect inflammation around the circumference of the implant.
To view device options go here.
REFERENCES:
- ASPS. “Report of the 2017 Statistics.” American Society of Plastic Surgeons (ASPS). 2018. Available: https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgerystatistics-report-2017.pdf
- Brown S. Lori Epidemiology of Silicone-Gel Breast Implants, Epidemiology: May 2002 – Volume 13 – Issue 3 – p S34-S39.
- Codner MA, Mejia JD, Locke MB, et al. A 15-year experience with primary breast augmentation. Plast Reconstr Surg. 2011 Mar;127(3):1300-10.
- Cohen Tervaert JW, Colaris MJ, van der Hulst RR. Silicone breast implants and autoimmune rheumatic diseases: myth or reality. Curr Opin Rheumatol. 2017 Jul;29(4):348-354.
- de Boer M, van Leeuwen FE, Hauptmann M, et al. Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast. JAMA Oncol. 2018;4(3):335-341.
- Doren EL, Miranda RL, Selber JC, et al. U.S. Epidemiology of Breast Implant–Associated Anaplastic Large Cell Lymphoma, Plastic and Reconstructive Surgery: May 2017 – Volume 139 – Issue 5 – p 1042-1050.
- FDA. Recommendations for “Saline, Silicone Gel, and Alternative Breast Implants.” See at: https://www.fda.gov/media/71081/download
- Frame JD. Commentary on: Breast Implants and the Risk of Breast Cancer: A Meta-Analysis on Cohort Studies, Aesthetic Surgery Journal, Volume 35, Issue 1, January 2015, Pages 63–65.
- Marano AA, Henderson PW, Prince MR, et al. Effect of MRI on breast tissue expanders and recommendations for safe use. J Plast Reconstr Aesthet Surg. 2017 Dec;70(12):1702-1707.
- Mona, https://fivethirtyeight.com/features/dear-mona-what-percentage-of-women-have-breast-implants
- Noels EC, Lapid O, Lindeman JH, Bastiaannet E. Breast implants and the risk of breast cancer: a meta-analysis of cohort studies. Aesthet Surg J. 2015 Jan;35(1):55-62.
- Pawluk W and Layne CJ. Power Tools for Health: how magnetic fields (PEMFs) help you. Publ. Friesen Press, 2017.
- Silver H. Reduction of capsular contracture with two-stage augmentation mammaplasty and pulsed electromagnetic energy (Diapulse therapy). Plast Reconstr Surg. 1982 May;69(5):802-8.
- Stewart PS, Bjarnsholt T. Risk factors for chronic biofilm-related infection associated with implanted medical devices. Clin Microbiol Infect. 2020 Aug;26(8):1034-1038.
- Tehrani K. What is capsular contracture and how can it be treated? https://www.plasticsurgery.org/news/blog/what-is-capsular-contracture-and-how-can-it-be-treated.
- Thimmappa ND, Prince MR, Colen KL, et al. Breast Tissue Expanders with Magnetic Ports: Clinical Experience at 1.5 T. Plast Reconstr Surg. 2016 Dec;138(6):1171-1178.