PEMF'S AND GALLBLADDER DISORDERS
Table of Contents
Gallbladder disorders (GBDs) affect 20 – 25 million Americans. These GBDs are typically costly to manage, with a $6 billion dollar cost to society every year in the US. GBD’s are a major cause of hospitalizations.
In 2004, there were 1092 GBD related deaths in the US, and about 80% of people who die of GBD never had prior pain or complications related to GBD. People who have “silent” gallstones will eventually develop problems, about 10% of them will over the next 5 years. About 1 – 2% of people with GBDs per year develop major gallstone complications.
The primary treatments for GBDs are painkillers and removing the GB, cholecystectomy. But there are other treatments that may be able to prevent or delay GB problems or complications. PEMF therapy is one of the most important ways to prevent GB disease that would otherwise result in surgery. We can say this based on the most recent understanding about how GBDs develop.
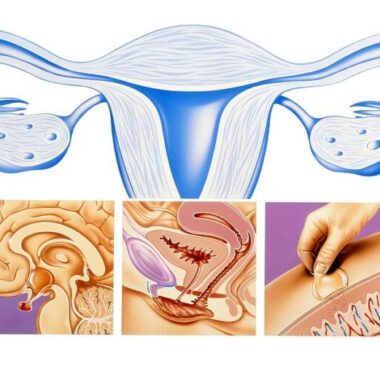
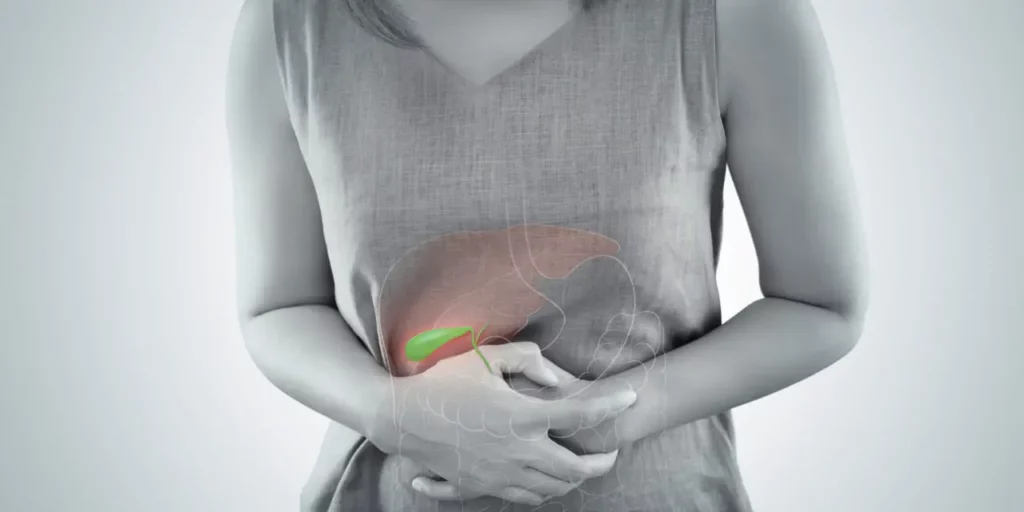
NORMAL GALLBLADDER FUNCTION
The primary function of the GB is to store and concentrate bile (also called gall, hence gallstones), a yellow-brown digestive juice continuously produced by the liver, amounting to about 10 – 30 ounces per day. The bile in the intestinal tract breaks down dietary fats and emulsifies them, allowing for the absorption of smaller fat molecules from the bowel into circulation. Bile contains mostly water, fats, cholesterol, salts, and bilirubin.
The bile normally produced by the liver is diluted and is not very effective in breaking down fats in the food. As a result, the body has adapted itself to concentrate the normally produced bile by diverting it to the GB. Only about 10% of the bile normally draining from the liver ends up in the bowel without being concentrated. Concentrated bile is much better at breaking down fats in our food, allowing better absorption of the dietary fats for use as energy. The GB removes water from this bile to make it 3-10 times more concentrated.
In order for the bile in the GB to do its job, it must be released by “squeezing the bag”, squirting the contents into the intestinal tract. GB contractions are part of the three phases of the digestive process: brain, stomach, and duodenal. (Behar) The brain phase starts as people are exposed to the smell, sight and taste of food. 30–40% of GB bile may be emptied at this phase. Stretching of the stomach (duodenal phase) by food triggers a vagal nerve GB reflex and release of cholecystokinin [CCK]. Most of the rest of the GB contents are emptied during this phase. Food containing fat entering the digestive tract stimulates CCK from the upper small bowel. CCK causes the GB to contract and release the bile.
Between feedings the GB has milder rhythmic contractions, some of which squeeze out bile like a rolling drum to help keep the bile in solution, preventing precipitation. Precipitation of bile contents, particularly cholesterol, can lead to chronic GB inflammation [chronic cholecystitis] and gallstone formation.
DEVELOPMENT OF GALLBLADDER DISORDERS
There are many risk factors for cholesterol gallstone formation. Some are modifiable and some are not. Non-modifiable risk factors include ethnic background, increasing age, being female, and family history or genetics. Modifiable risk factors for GBD are obesity, rapid weight loss, and a sedentary lifestyle. Risk factors for biliary sludge, which often leads to gallstones and can be painful and lead to the removal of the GB, include pregnancy; drugs like ceftriaxone, octreotide, and thiazide diuretics; and total parenteral nutrition or fasting. Intermittent fasting may also be a predisposing situation. Some diseases are risk factors for black pigment gallstones including cirrhosis, chronic red blood cell destruction (hemolysis), and Crohn’s disease. GBD in childhood, once rare, is increasing with similar risk factors as in adults, especially obesity.
Diets specifically high in cholesterol, fatty acids, carbohydrates, or legumes seem to increase the risk of cholelithiasis. On the other hand, unsaturated fats, coffee, fiber, vitamin C/ascorbic acid calcium, and moderate use of alcohol reduce the risk.
Reduced physical activity heightens the risk of gallstone disease whereas increased physical activity helps prevent gallstones, independent of weight loss. Increased endurance exercise (up to 30 minutes 5 times a week) may prevent symptomatic gallstones from developing in men.
There is a concept of lithogenic [stone-forming] bile. Stone forming bile is the most likely to precipitate cholesterol crystals in the GB, which often leads to chronic inflammation and gallstones. The problems stem from bile supersaturated with cholesterol. Supersaturated GB cholesterol creates a multitude of reactions in the GB. Supersaturation happens when the GB doesn’t properly contract and expel its bile. As bile sits in the GB for prolonged periods, the water is extracted from it causing excess concentration or precipitation of cholesterol crystals.
The GB may have decreased contractility for other reasons, but this could also be caused by the presence of high levels of cholesterol crystals. These accumulated cholesterol crystals embedded in the wall of the GB leading to GB inflammation and hence further decreases in contractility. Decreased contractility further leads to decreased expulsion of bile into the intestine. In other words, a vicious cycle is set up.
Since fat is necessary to stimulate GB contractions the problem is further complicated by currently popular low-fat diets, which do not cause enough GB stimulation. The situation is made even more challenging because people often don’t drink enough water/fluids and/or drink too many stimulants, such as coffee, colas, or tea, that cause increased urine fluid loss.
High levels of cholesterol in the diet also impair small intestinal muscle cell contractility, slowing intestinal transit. This slower transit increases small bowel bile deoxycholic acid accumulation, resulting in even greater cholesterol absorption. Both of these actions increase inflammatory cells in the bowel wall and also thicken the GB wall muscle. In animal studies these abnormalities took place even four weeks after being fed a high cholesterol diet, leading to gallstones being formed.
Both gallstones and abnormalities of the GB wall tissue and muscle are caused by stone forming, high cholesterol bile. These can develop independently of each other, even though they may be detected simultaneously in people who don’t have symptoms. Cells exposed to lithogenic bile have increased inflammation that stimulates mucus secretion way before gallstones are formed. So, inflammation is a common predisposing factor to the development of chronic inflammation of the GB, cholecystitis, and gallstones. This inflammatory process worsens over time due to the continuous entry of bile salts into an already inflamed, diseased GB.
Lithogenic bile and GB disease is higher in females, suggesting that sex hormones may be involved. Estrogens play a big role in developing GBD because they increase liver production and secretion of cholesterol into the bile.
GB PAIN
GB pain can be caused by chronic inflammation [cholecystitis], acute cholecystitis, sludge, or gallstones.
CHRONIC CHOLECYSTITIS
There may have been repeated episodes of acute inflammation, variably symptomatic, clear or vague, potentially leading to the diagnosis of chronic cholecystitis.
ACUTE CHOLECYSTITIS
Acute cholecystitis usually results from an acute pain event diagnosed without any previous evidence of GBD. Even in this setting, upon further diagnostic workup, it will be discovered that there has been an underlying longer-term, smoldering, process of GB dysfunction, and inflammation.
GB SLUDGE
Individuals with GB-like pain will often show sludge on ultrasound. Sludge is indicative of accumulated concentrated bile. This sediment consists of cholesterol crystals, calcium bilirubinate pigment, and other calcium salts. Sludge is common in pregnancy; with rapid weight loss, particularly in the obese; with a critical illness involving low or absent oral intake and the use of total parenteral nutrition (TPN); and following gastric surgery. It can have associated biliary stones with common bile duct obstruction, and with bone marrow or solid organ transplantation. The clinical course varies. Sludge often vanishes, particularly if whatever is causing it is resolved. At other times, sludge waxes and waned, and some become gallstones. Complications caused by sludge include biliary colic, acute liver inflammation (cholangitis), and acute pancreatitis.
GALLSTONE PAIN
Gallstone pain is typically steady, severe, located in the upper abdomen or radiating to the back, lasts more than 30 minutes, happens periodically, is often associated with nausea and vomiting, and frequently follows fatty meals by 30-90 minutes. This is commonly called biliary colic. By contrast, acid-related pain, often with duodenal or peptic ulcers, is more often improved with food.
FUNCTIONAL GBD
Functional disorders of the GB are difficult to define. GB muscle function (motility) abnormalities (dysmotility) may be caused by metabolic abnormalities or by a motility disorder on its own. The pain of GB dysfunction is similar to chronic cholecystitis. Functional GBD includes episodes of moderate-to-severe steady pain located in the stomach area or right upper abdomen that last at least 30 minutes, usually not following meals nor occurring daily. Functional GBD should only be considered after gallstones and other anatomical abnormalities have been excluded.
CHOLECYSTITIS
Inflammation of the GB [cholecystitis] can be either acute or chronic.
CHRONIC CHOLECYSTITIS
Chronic cholecystitis is the most common cause of gallstones developing. It is a slowly progressive process, developing over years, and when it becomes suddenly symptomatic, gallstones are discovered in a workup. In other words, the presence of gallstones is evidence of significant, but not necessarily detectable, GB inflammation and dysfunction that has been present for a long time, often years.
ACUTE CHOLECYSTITIS
Acute cholecystitis most frequently involves the sudden impaction of gallstones in the GB outlet. Chronic cholecystitis is the most common risk factor for acute cholecystitis. Gallstones are not always present in cholecystitis. In this case, the inflammation has reached the point of causing significant distress leading to the diagnosis. However, in the presence of stones, especially obstructing stones, pressure in the GB increases, the organ becomes enlarged, the GB wall thickens, the GB blood supply significantly decreases, and a discharge from the GB wall may form.
There may have been repeated episodes of acute inflammation, variably symptomatic, clear or vague, potentially leading to the diagnosis of chronic cholecystitis. The GB can become infected by various bacteria, including those that are gas-forming. And in more extreme cases, an inflamed GB can undergo cell death and infectious gangrene. If left untreated this may progress to symptomatic sepsis. Failure to properly treat acute cholecystitis may result in perforation of the GB, a rare but life-threatening phenomenon.
Acute cholecystitis also can be associated with gallstone pancreatitis. If gall stones dislodge from the GB, enter the cystic duct, move down to the sphincter of Oddi and are not cleared, blocking the pancreatic duct, this sequence of events can cause a backup of pancreatic and biliary secretions, ending in pancreatitis. Pancreatitis is a serious medical emergency.
GALLSTONES
While gallstones in GBD are easier to detect, a functional form of GBD, called functional or acalculous GBD, may be harder to diagnose. Another name for this is biliary dyskinesia. The pain may be caused by obstruction at the GB outlet, incoordination between GB contractions and the sphincter outlet of the bile duct to the duodenum (sphincter of Oddi), or even visceral hypersensitivity. This is usually diagnosed by a GB emptying study using cholecystokinin, the hormone the body produces to cause the GB to contract.
Gallstones are hard, pebble-like structures that can block the duct leading from the GB, the cystic duct. This is a relatively passive fluid drainage system. The ducts leading from the liver and the GB do not contract to move the fluid along. At the end of this drainage system is the sphincter of Oddi, a muscular gatekeeper or valve, which opens and closes to allow bile and pancreatic fluids to drain into the duodenum.
The formation of gallstones is often preceded by the presence of biliary sludge. In the U.S., most gallstones consist largely of bile supersaturated with cholesterol. This super-saturation, which results from the cholesterol concentration being so great that it can’t be kept in solution, is caused primarily by excess production of cholesterol by the liver. This excess cholesterol in the GB can form cholesterol crystals, which can embed themselves in the GB wall creating chronic inflammation. One of the common contributing factors to crystallization is relative dehydration.
Loss of GB muscular-wall contractility and excessive contractility of the sphincter of Oddi, which controls the flow of bile to the duodenum, are also involved in gallstone formation. This low contractility leads to bile staying in the GB too long (delayed GB emptying), leading to continuous accumulation of excess bile and the compounding risk for stone formation.
There is increasing evidence that gallstones, although important in the cause of bile duct complications, do not play a significant role in the development of cholecystitis. It’s the other way around.
FUNCTIONAL GBD
GB ultrasound can rule in or out lithogenic bile with microcrystals. The diagnosis is made by seeing decreased GB ejection fraction on a nuclear scan study following intravenous cholecystokinin (CCK) and after resolution of this biliary pain if the GB is removed.
This diagnostic workup does not tell you the cause of the functional GB problem. GBs with lithogenic bile have a lower ejection fraction after CCK or meal stimulation. Microscopically these GBs show inflammation consistent with chronic cholecystitis. Functional GBD should not show cholecystitis or lithogenic bile with excess cholesterol. This testing is rarely done, because to detect the presence of lithogenic file with excess cholesterol requires an invasive procedure.
LIVING WITHOUT A GB
The standard medical solution to GB disease is cholecystectomy, or surgical removal of the GB. This is considered common “garden-variety” surgery, but removing the GB creates its own risks. These are not only the surgical risks associated with cholecystectomy, whether through laparotomy or laparoscopy, but also the nutritional and physiologic changes that happen in the body as a consequence.
Following GB removal several problems frequently arise:
- poor fat digestion
- bile reflux gastritis
- bile reflux esophagitis
- difficulty swallowing and regurgitation
- interference with normal stomach acid functions
- sphincter of Oddi dyskinesia
The lack of a GB clearly affects digestion because concentrated bile is no longer available to help with fat digestion. Fats are important to physiologic and nutritional function, as they were before GB disease and after removal of the GB.
In addition, one of the most common consequences of removing the GB is bile reflux gastritis. Bile reflux into the stomach happens in about 80%-90% of people after GB surgery. Bile reflux is alkaline.
Therefore, alkaline bile reflux is a contributing factor for chronic esophagitis or Barrett’s esophagus. (Uyanikoglu). Esophageal reflux symptoms are seen in about 40% of people after cholecystectomy, similar to the rates reported in the general population.
Abdominal pain, bloating and nausea are as common in those with alkaline bile reflux as in those with the more common acid reflux. Other symptoms include difficulty with swallowing and regurgitation. In addition, since bile reflux is alkaline, it reduces the normal acidity required by the stomach to do its proper tasks in breaking down food, destroying microbes in the stomach and producing vitamin B12.
SPHINCTER OF ODDI DYSKINESIA (SOD)
SOD creates symptoms that are biliary-like but do not develop until the GB has been removed. These individuals have symptoms and signs suggestive of transient bile duct obstruction, and those of pancreatic SOD are associated with elevation of pancreatic enzymes and even full-blown pancreatitis.
There are 3 types of SOD. Those with type I SOD complain of biliary-like pain, have elevated liver function tests documented on two or more occasions, a dilated common bile duct with a diameter equal to or greater than 12 mm, and delayed contrast drainage from the common bile duct tested by endoscopic retrograde cholangio-pancreatography (ERCP) and basal pressures higher than 40 mm Hg. Type II have biliary-like pain and only one or two of the previously mentioned criteria. Type III are characterized by recurrent biliary type pain but without laboratory or pressure testing abnormalities.
Most symptoms with type I dyskinesia respond to cutting the sphincter muscle (sphincterotomy). Most with type II SOD also improve after sphincterotomy, but fewer respond than with type I. Type III’s have biliary-like pain but normal laboratory tests and SOD pressures. Most do not respond to sphincterotomy, suggesting that the pain is caused by gastrointestinal functional disorders unrelated to the SOD.
ROLE OF PEMFS IN GBD
GB disease appears to start with excessive bile cholesterol levels, excess lithogenic bile accumulation, decreased bile expulsion with fatty meals, and possible relative dehydration. These factors all lead to accumulation of cholesterol crystals that cause significant increases in GB inflammation. This sequence of events eventually leads to inadequate elimination of the normally concentrated GB bile, accumulation of bile/cholesterol sludge and eventual formation of cholesterol stones. Part of this process also causes the normal GB contractions to dysfunction further accumulating sludge and cholesterol crystals. When sludge, stones and inflammation lead to enough GB irritability, biliary colic ensues, even without the presence of gallstones blocking the outlet of the GB. Additional consequences of these processes are gallstones and/or biliary duct stones. These stones can lead to possible jaundice from bile duct obstruction and pancreatitis from pancreatic duct obstruction.
Therapeutic strategies would therefore be to decrease liver cholesterol production, increase GB bile expulsion, increase hydration, decrease GB inflammation, and reduce GB irritability causing dyskinesia and colic.
PEMFs can be helpful through all the phases of GB disease. Usually multiple preventative and treatment strategies are necessary. No single treatment strategy is going to be perfectly effective.
PEMFS CAN DECREASE CHOLESTEROL PRODUCTION
Decreasing cholesterol production by using anti-cholesterol drugs creates new problems since cholesterol is naturally produced by the body and is necessary for many metabolic processes. So, aggressive pharmacological disruption of cholesterol production is not natural. Nutritional approaches to decreasing cholesterol production would be more natural. Decreasing cholesterol production naturally while at the same time while following multiple additional strategies would be a comprehensive way to deal with cholesterol issues.
Evidence for the value of PEMFs in reducing cholesterol comes from both animal and human studies. Among the animal studies, a 60 Gauss magnetic field applied for one hour with frequencies ranging between 12 – 460 Hz, reduced cholesterol levels by 9 – 12% and triglyceride levels by 16 – 18% at 24 hours after exposure. (Bellossi) However, in a time sequence study, cholesterol and triglyceride concentrations increased at 3 and 8 hours, then decreased at 24 hours, followed by a return to normal after 48 and 96 hours, respectively.
Decreased physical activity appears to increase cholesterol levels. PEMFs have been found to impact cholesterol levels in normally exposed rats as well as in rats with limited mobility. (Temur’iants) Exposure was with .05 gauss at 8 Hz, 3 hours a day for 45 days. Magnetic field exposure alone without decreased mobility had no effect on lipid metabolism at this level of intensity and exposure. However, the PEMF prevented lipid elevation in the mobility-limited rats.
It appears that the PEMF treatment of blood, autohemotherapy, studied in Belarus (Ostapenko) also decreases cholesterol and triglyceride levels, in addition to other cardiovascular benefits in individuals with disseminated atherosclerosis, using 10 Hz at about 150 Gauss. This is akin to hemodialysis where the blood passing through a filtration machine is exposed to the PEMF field, before being passed back into the body.
In another study in rats, (Sieron) 40 Hz PEMF from 20 – 150 Gauss, significantly increased bile secretion, with greater secretion levels as the field intensity increased.
PEMF TREATMENT OF GB DISEASE
In Russia, PEMFs have been used successfully in the treatment of various aspects of GB disease. (Grigorev) One treatment approach has been to use a PEMF applicator positioned over the GB area, at 50 Hz, 300-400 Gauss for 10-20 min. daily. PEMF Treatments promoted recovery in biliary duct diseases, improved motor function of biliary sphincters and bile outflow considerably decreased inflammation and pain, and were especially helpful in GB hyperkinesia and sphincter spasm.
A study in China (Deng) in individuals undergoing rehabilitation for recovery from stroke, using 60 Hz PEMFs, found that total cholesterol and triglycerides levels dropped significantly.
Using a different technology (Seqex), 143 patients with musculoskeletal disorders had ELF magnetic treatments using the Seqex device, using various complex frequencies at about 0.1 Gauss over 10 treatments had stabilization of cholesterol levels. (Ciafoni) On the other hand, when the same device was used in healthy individuals there were no significant effects on cholesterol levels. (Vallesi) It is not uncommon for individuals with other health conditions to have elevated cholesterols.
THE EFFECTS OF PEMFS ON INFLAMMATION
The effects of PEMFs on inflammation are well-known and are better explained here and in the book, Power Tools for Health. The benefits of PEMFs on inflammation associated with GBD would be expected to be no different than those associated with any other health conditions. In other words, PEMFs should be significantly helpful in decreasing GB related to chronic inflammation and pain and should well be considered the first step in the management of GBD.
With biliary sludge, removing the cause is probably the most important factor, especially through increasing hydration, decreasing cholesterol levels in the bile, and helping GB contractions. Because inflammation is almost always present when there is biliary sludge, PEMFs may be very helpful to decrease symptoms until the causes and the sludge are removed.
HELP WITH GALLBLADDER MOTILITY
When there is excessive gallbladder muscle irritability, a major cause of GB symptoms, the muscle relaxing and natural pain-relieving effects of PEMFs are also well known and covered in the book Power Tools for Health. Because PEMFs offer a significant benefit for pain caused by both inflammation and GB muscle spasm, they are valuable in reducing and preventing GB pain.
PANCREATITIS ASSOCIATED WITH GBD
The treatment of pancreatitis caused by obstructing GB stones is best dealt with by urgently removing the obstructing stones, as this can be a medical emergency. Once the obstructing threat is removed, recovery from pancreatitis may be greatly helped with PEMF therapy by decreasing the severe inflammation in the pancreas caused by the destructive effects of pancreatic enzymes being released into the pancreatic tissues. The same principles that are applied to the treatment of inflammation anywhere else in the body by using PEMFs would apply here. In this situation PEMF therapy may need to be used continually until the inflammation subsides and the pancreas is determined, through blood testing and decreased symptoms, to be healed.
ACUTE CHOLECYSTITIS
Acute cholecystitis is likewise considered a potentially life-threatening medical emergency and needs to be treated aggressively with antibiotics and possibly with cholecystectomy. The role of PEMFs in this setting is best to help with recovery from surgery.
PREVENTING GALLBLADDER CANCER
Gallbladder cancer (GBC) is another form of GBD. The primary risk factors for GBC are chronic gallstones. Probably the leading cause is a chronic inflammation of the gallbladder with calcium crystals being deposited in the gallbladder wall. Gallbladders with partial calcifications are considered premalignant and should be removed preventively. Chronic bacterial GB infections may also increase the risk of gallbladder cancer. It is difficult to diagnose, usually discovered at a late stage, and has a dismal prognosis. The overall mean survival rate for gallbladder cancer is 6 months with a five-year survival rate of 5%. So, again, since PEMFs have a critical role in reducing chronic GB inflammation, they would be very helpful in preventing GBC.
SUMMARY
GB disease (GBD) has multiple facets to it. Most of the time it is associated with abnormal accumulation of cholesterol crystals, chronic inflammation, and challenges with GB muscle function. If a sufficient amount of cholesterol crystals accumulate over time, the GB does not get rid of this concentrated bile appropriately and GB sludge can begin to develop, leading to gallstones. Gallstones can lead to cholecystitis and, if they are ejected into the biliary system, can lead to obstructions causing jaundice or pancreatitis.
The proper management of GBD is to decrease the amount of cholesterol concentrating in the GB, facilitating regular elimination of bile from the GB, decreasing the concentration of the bile, and reducing the risk of inflammation. The most logical approach to GBD is prevention, followed by reduction in risk of progression of inflammation, and followed by aggressive nonoperative management. GB surgery should be considered a last resort, except in the presence of a life-threatening condition. GB surgery, while considered a rescue therapy, creates its own complications long-term, which is why nonsurgical therapeutic approaches become important.
PEMF therapy early in the course of GBD can be extraordinarily helpful in mitigating symptoms and preventing progression. It may also be especially useful in GB disease that does not involve gallstones. At this point, it is not known whether PEMF therapies, along with other strategies may decrease gallstones, especially early forming stones. It may be appropriate to consider PEMF therapy preventively to the GB area in anybody with significantly elevated cholesterol levels until cholesterol levels can be reduced.
References
- Behar J. Physiology and Pathophysiology of the Biliary Tract: The GB and Sphincter of Oddi—A Review. February 2013. ISRN Physiology 2013(4).
- Bellossi A, Pouvreau-Quilien V, Rocher C, et al. Effect of pulsed magnetic fields on triglyceride and cholesterol levels in plasma of rats. Panminerva Med 40(4):276-279, 1998.
- Ciafaloni A. Cyclotronic ion resonance therapy and arthralgia. Electromagn Biol Med. 2007;26(4):299-303.
- Deng AW, Yuang XG, Wei D, et al. Effect of power-frequency electromagnetic fields on stroke during rehabilitation. Di Yi Jun Yi Da Xue Xue Bao. 2004 Aug;24(8):946-9, 952.
- Grigorev KI. Nondrug treatment of chronic digestive system diseases in children. Pediatriia (9):85-93 1991.
- Ostapenko VA, Kruchinsky NG, Teplyakov AI, et al. The extracorporeal of low-level alternating pulsing magnetic fields (autohaemomagnetic therapy) at patients suffering from disseminated atherosclerosis: the first experience and effects (meeting abstract). European Bioelectromagnetics Assoc. (EBEA), 4th International Congress, 19-21 November, Zagreb, Croatia, 1998.
- Sieron A. The metabolism of bile acids in experimental animals under the influence of variable magnetic fields – different inductions (meeting abstract). European Bioelectromagnetics Association (EBEA), 3rd International Congress, 29 February-3 March, Nancy, France, 1996.
- Stinton LM, Shaffer EA. Epidemiology of GB disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172-187.
- Temur’iants NA, Evstaf’eva EV, Makeev VB. Correction of lipid metabolism in rats with limited mobility by an alternating magnetic field of infra-low frequency. Biofizika 30(2):313-316, 1985.
- Uyanikoglu A, Akyuz F, Ermis F, et al. Does Cholecystectomy Increase the Esophageal Alkaline Reflux? Evaluation by Impedance-pH Technique. J Neurogastroenterol Motil. 2012;18(2):187-193.
- Vallesi G, Raggi F, Rufini S, et al. Effects of cyclotronic ion resonance on human metabolic processes: a clinical trial and one case report. Electromagn Biol Med. 2007;26(4):283-8.